What's the right plan for you?
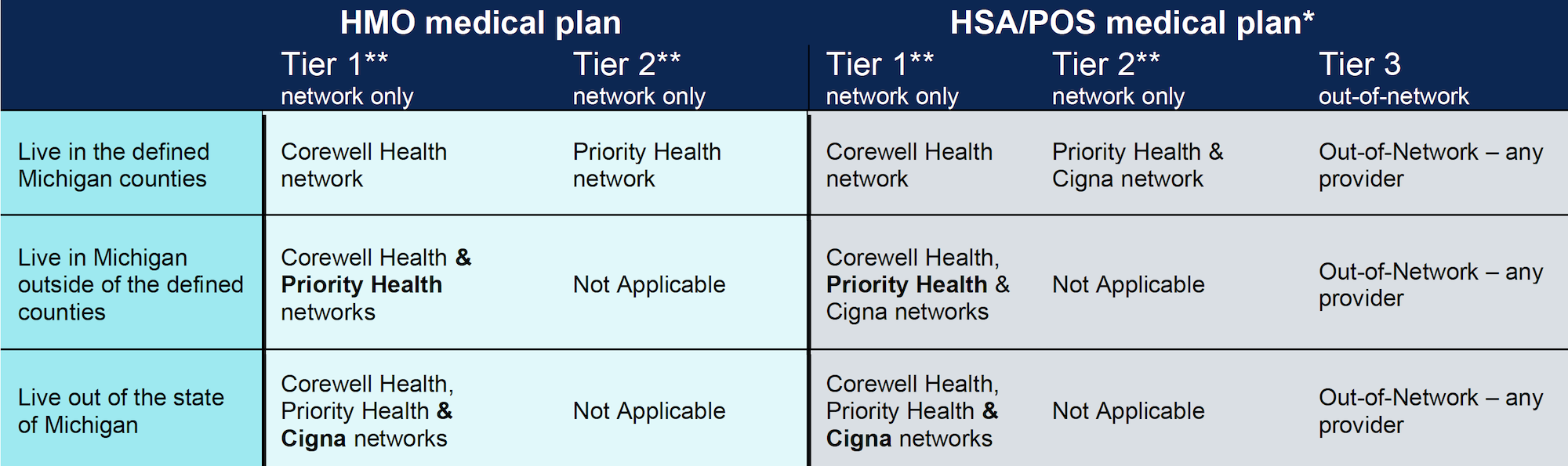
Medical plan coverages are based on plan selected, where you live and which provider you select. Your medical plan offering is based on your home address listed in Workday.
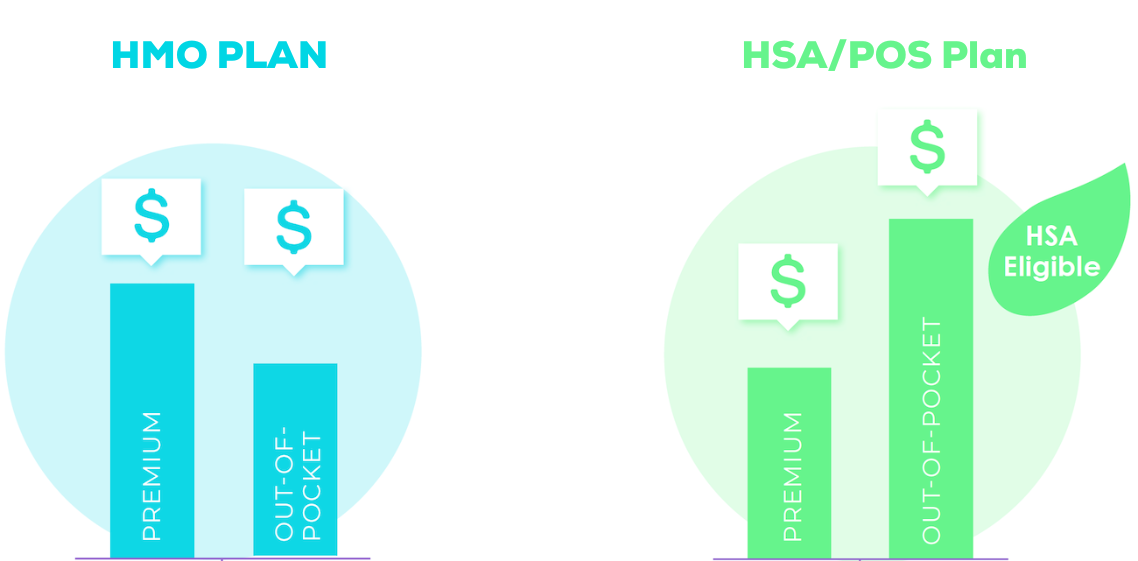
- The HMO Plan For those who prefer a lower deductible but higher team member contributions.
- The HSA/POS Plan Available for those who might be looking to make a minimal team member contribution but pay more at point of service with higher deductibles.
What will you pay for your medical plan?
Your medical premiums depend on the plan you choose, the coverage you elect, your common law employer and your full-time or part-time status.
HMO Plan
This plan offers higher premiums and lower out-of-pocket costs. Costs are lowest when members receive care at Corewell Health facilities and providers; there is no out-of-network coverage.
HSA/POS Plan
This high-deductible health plan balances lower premiums with higher out-of-pocket costs and out-of-network coverage. Corewell Health helps offset these costs when you fund a Health Savings Account.
HMO Plan |
HSA/POS Plan |
|
|---|---|---|
Your Premium Cost |
$$$ |
$ |
Deductible Tier 1 |
$650 individual, $1,300 family |
$1,600 individual, $3,200 family |
Deductible Tier 2 |
$2,000 individual, $4,000 family |
$2,000 individual, $4,000 family |
Deductible Out-of-Network |
Not covered |
$5,000 individual, $10,000 family |
Health Savings Account |
No |
Corewell Health contributes up to $500 individual/ $750 family |
* except in cases of emergencies or cases in which Priority Health has approved care outside of the network.
Network and Providers
Both of our medical plans offer lower out-of-pocket costs at Corewell Health facilities, providers, and services. You also have access to the Priority Health network.
Tiers are not something you enroll in or are locked into – it’s how your coverage and deductible is applied, based on where you choose to receive your care and the provider you select.
Navigating Tiers In Your Medical Plan
Understanding Tiers: What If I'm Referred To A Tier 2 Facility?
What Happens If My Primary Care Doctor Is In Tier 2?
What Happens If I Need A Hospital-based Service (like an X-Ray?)
What Happens If I Need Hospitalization?
Understanding Tiers: What If I Need Emergency Care?
(Or My 4-Legged Family Member Needs Emergency Care?)
Corewell Health Services
Tier 1: Corewell Health facilities across Michigan including legacy Beaumont Health, Lakeland and Spectrum Health and providers, Answer Health, BACO, Holland Hospital facilities and providers, We Are for Children, as well as affiliated ancillary facilities such as Mary Free Bed, Pine Rest and Forest View.
Tier 1 providers may refer to Tier 2 facilities/providers. You are encouraged to contact Priority Health Customer Service to confirm benefits prior to engaging in services.
If you live out-of-area*: You'll receive Tier 1 coverage no matter where you receive your health care, as long as you're still in the Priority Health network.
Tier 1 includes all Priority Health facilities and providers. If you live outside of Michigan, you have access to both the Priority Health and Cigna networks in whichever plan you choose.
Priority Health
Tier 2: The Priority Health network includes all other Priority Health participating facilities and providers.
Out-of-Network Care
Tier 3 (HSA/POS Only): Care outside of the Priority Health network is only covered on the HSA/POS Plan, with higher out-of-pocket costs.
Because of this, before visiting a new provider or facility, confirm that they participate in the Priority Health network.
PriorityGPS
Priority Health has partnered with Accolade, a care delivery, navigation and advocacy services company, to offer you PriorityGPS. PriorityGPS gives you and your family access to personalized support from a Health Assistant and nurse for all your healthcare and benefits questions. You can also view all your benefits in one place with the Accolade member portal and mobile app. PriorityGPS helps to make healthcare easier for you to navigate. PriorityGPS can be reached at 866-518-1769 and is the one-stop-shop for all your Priority Health customer service and benefits questions. You can also text at ACCD01 to connect with a Health Assistant.
Through one point of contact you can access:
- Health care navigation and advocacy – including appointment scheduling, guidance to high-value providers, and treatment decision support.
- Benefits and coverage guidance – including cost estimation, prior authorization, claims processing, coverage and other employer benefits-related questions.
- Condition management and prevention – including nurse triage, virtual care, expert second opinion, proactive and targeted clinical interventions.
PriorityGPS 2nd.MD program
2nd.MD provides members with a third-party second opinion for complex treatment plans including procedures, surgeries, and other medical situations. 2nd.MD is a nationwide second medical opinion service that offers an external third-party review of a member’s treatment plan by a leading provider with the goal of providing members additional objectivity, credibility, and confidence in treatment. Corewell Health members targeted for a second opinion will receive email and phone outreach from 2nd.MD representatives on behalf of the PriorityGPS offering.
Riders on the Corewell Health Medical Plan
Expanded infertility rider
Currently, all Priority Health medical plans cover diagnostic, counseling, and planning services for the treatment for the underlying cause of infertility and prescription drugs used for the purpose of treating infertility. Examples of covered services include endometrial biopsy, diagnostic laparoscopy or hysteroscopy, hormone evaluation, and semen analysis.
The expanded infertility rider provides coverage for assisted reproduction and artificial conception services regardless of provider participation. Examples of covered assisted reproduction and artificial conception services include within the expanded rider: Sperm count, egg freezing, thawing and storage, in vitro fertilization (IVF), artificial insemination (AI) and services associated with the treatment and underlying conditions of assisted reproduction and artificial conception such as ultrasounds and imaging. Services specific to this rider have a $50,000 lifetime maximum benefit.
Habilitation coverage rider
This rider provides coverage for habilitation services which are defined as those health care services that help a person keep, learn, or improve skills and functioning for daily living e.g., therapy for a child who isn’t walking or talking at the expected age.
All of the following must be met for coverage of habilitative services not related to autism spectrum disorder:
- Treatment must be evidence-based physical or occupational therapy provided by an appropriately licensed therapist under the direction of a physician or advanced practice nurse in accordance with a written treatment plan established or certified by the treating physician or advanced practice nurse.
- One of the following diagnoses:
- Developmental delay
- Developmental coordination disorder
- Mixed developmental disorder
- Developmental speech or language disorder
Lab coverage for CBC, CMP and Vitamin D
CBC, CMP and/or vitamin D labs at 100% prior to deductible with the HMO plan and 100% after the deductible with the HSA/POS plan.
Cranial Prosthesis Rider
This coverage rider provides coverage for cranial prosthesis for hair loss due to a medical condition as described in the Priority Health schedule of copayments and deductibles. Cranial prosthesis (wig, toupee, headband) is covered when performed by a health professional.
Finding a Priority Health Provider
To find in-network providers under
your plan, visit priorityhealth.com.
First, select the Find a Doctor tool. Under the employer plan section, select Corewell Health Employer Group.
Out of area team members: Select the Find a Doctor tool. Under the plan dropdown menu, select:
- PriorityHMO for the HMO Plan
- PriorityPOS A for the HSA/POS Plan
- Cigna: for members out of state
Finding a Corewell Health Provider
For a complete list of Corewell Health facilities, visit corewellhealth.org and scroll to "Our connected network of care." From there, you can select a region.
You are able to obtain services from either side of the system at Tier 1 coverage.