Who is eligible for benefits?
Full-Time
- Regular full-time team members who are scheduled to work 30 hours or more per week are eligible to enroll in all PDS Health benefit offerings.
- Temporary in-house full-time team members who are scheduled to work 30 hours or more per week are eligible to enroll in a PDS Health medical plan and the 401(k) plan.
Part-Time
- Regular part-time team members who are scheduled to work less than 30 hours per week are eligible to enroll in the PDS Health Dental, 401(k) and Voluntary Auto, Home, Pet and Legal plans.
- Temporary in-house part-time team members who are scheduled to work less than 30 hours per week are eligible to enroll in the 401(k) plan.
Need to Change Your Benefits?
Team members have 30 days from the date of hire or qualifying life event to enroll or make changes to benefits.
Eligible Dependents Include:
- Your legal spouse
- Your legally registered and valid domestic partner (RDP) (where state law and insurance carriers allow)
- Your dependent children until they are 26 years old. “Children” include you or your spouse’s/RDP’s biological children, step-children, adopted children, including children placed with you for the purpose of adoption, children for whom you are required to provide insurance coverage under a Qualified Medical Child Support Order (QMCSO), or disabled children who have reached the maximum age and who are (or become) physically or mentally incapable of self support (medical certification required)
Team members who cover dependents on a PDS Health medical, dental and/or vision plan will be required to verify dependent eligibility.
For more information on the dependent verification, refer to the Dependent Eligibility Verification flyer on PDSConnect.
When are team members eligible for benefits?
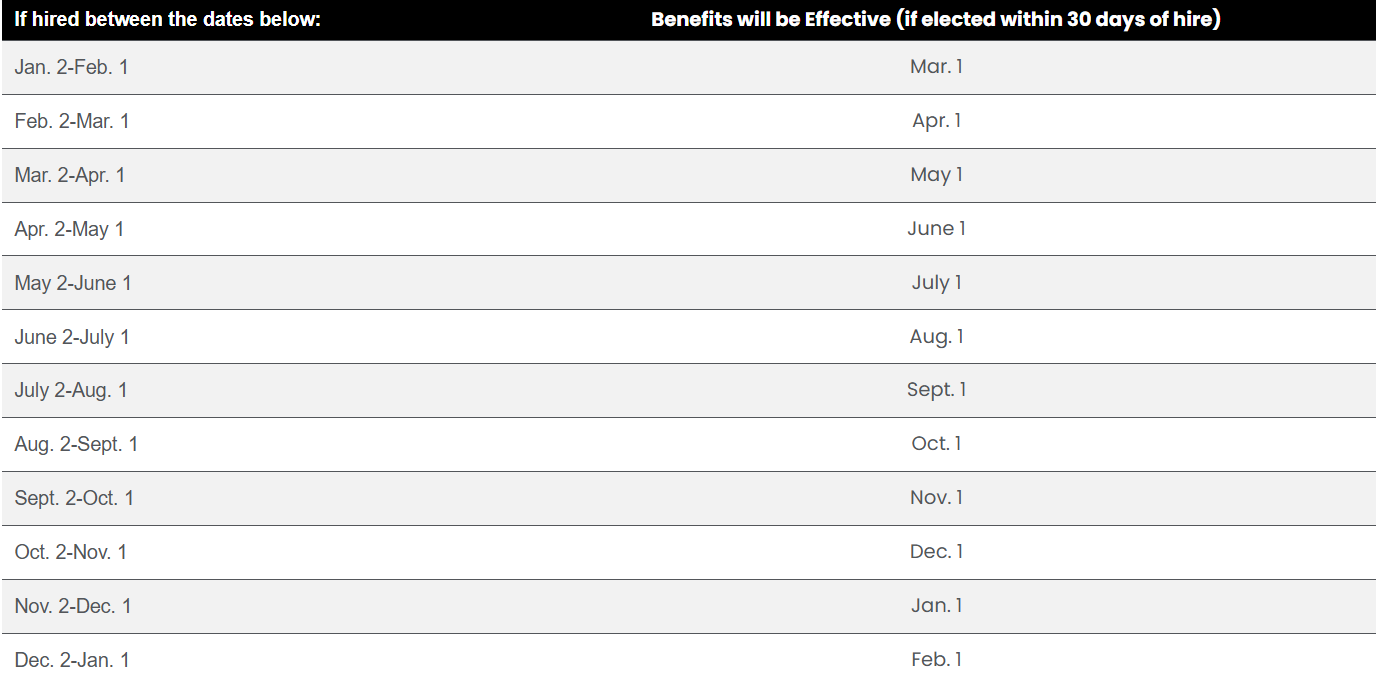
Your coverage will become effective on the first of the month following one month of continuous service, which includes any orientation period and new hire benefits eligibility waiting period. You must be actively at work for your coverage to be effective on your benefits eligibility date.
Qualifying Life Events
Other than during annual open enrollment, you may only make changes to your benefit elections if you experience a qualifying life event, including marriage, divorce, the birth/adoption of a child or gain/loss of other coverage. You have 30 days from the date of your qualifying life event to make changes to your benefit elections.
Visit the People Services Center and follow the steps in this Quick Reference Guide (QRG) to change your benefit elections. Alternatively, you can contact a Benefits Advocate at (877) 536-8693. If you miss the 30-day window you will need to wait until the next annual open enrollment to make changes. Financial hardship is not considered a qualifying life event and is not eligible for enrollment changes outside of your new hire or open enrollment window.
When you enroll a dependent in a PDS Health medical, dental, and/or vision plan, you must provide supporting documentation specified by PDS Health to verify that the individual(s) you have enrolled meet the eligibility requirements. For a more detailed list of eligible dependents and required documentation, check out the Dependent Eligibility Verification flyer on PDSConnect.
If you have questions regarding the enrollment process, or for questions regarding your specific benefits, contact a Benefits Advocate at (877) 536-8693 or pdsbenefits@aon.com, M-F 6:00 am to 4:00 pm PT.
Important Notice: This site provides information about the benefits and coverages that are available across the benefit plans maintained by PDS Health (“PDS®”) and by its PDS Supported Entities. This site applies to all team members. The term “team member” in this site refers to you, whether your employer is PDS® or a PDS Supported Entity. When the term “plan” or “Plan” is used in this site, it refers to the benefit plans that each employer makes available to its team members.
This site provides a general description of your employer’s benefits, and it serves as a summary of material modifications to the ERISA-required Summary Plan Descriptions applicable to these benefits (e.g., benefit booklet or evidence of coverage). This site does not describe all terms and conditions that may apply to your benefits. Details, including terms, limitations, and other conditions are provided in the ERISA plan document. If the information in this site differs from the ERISA plan document or Summary Plan Descriptions, then the ERISA plan document and Summary Plan Descriptions should prevail, as applicable.



